What is Sciatica?
Sciatic pain (commonly known as sciatica) is a symptom of nerve pain from an irritation of the sciatica nerve. The nerve starts in the lower back and extends through the gluteal area, the hamstrings and finally into the calf. You will hear sciatica spoken about as a condition, however it is a symptom. Similar to how you may have ‘Influenza’ with symptoms of coughing and sneezing – patients will have a ‘Disc Herniation’ with symptoms of ‘Sciatica’.
Anatomy of the Sciatic Nerve
The sciatic nerve is the thickest and longest nerve int he body. At it’s widest length it is actually almost the diameter of your finger. The nerve originates at ‘nerve roots’ in the lower back region. Two nerve roots originate in the lumbar spine region, while three nerve roots originate in the sacral region. These nerve roots combine to form one sciatic nerve down he leg. An injury directly to the sciatic nerve is actually rare, however tension or compression to the nerve due to a variety of factors is common.
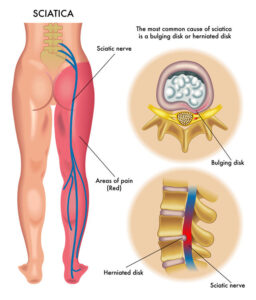
Figure 1. Sciatic Nerve Anatomy
What causes Sciatica?
Sciatica can be caused by a multitude of conditions, however most cause compression to areas of the sciatic nerve.
- Herniated Discs – a protruding disc in the lower spine can cause pressure on the nerve root
- Spinal Stenosis – is an abnormal narrowing the the spinal canal, usually due to osteoarthritis
- Spondylolisthesis – is where one vertebra has slipped forward above the vertebra below it
- Piriformis Syndrome – where tightness and spasms of a muscle in the deep glute muscles can pinch the nerve
- Tumor – in the lumbar spine or spinal canal
- Trauma – injury to the sciatic nerve or the lumbar spine
- Cauda Equina Syndrome – a serious and rare condition where the bundle of nerves at the bottom of the spinal cord is compressed, causing loss of bowel and bladder control. This is a medical emergency.
What are the risk factors?
- Previous injury – an injury to the lumbar spine in the past
- Age – as we get older, our tissue becomes less pliable and stiffer, which makes discs more prone to injury
- Overweight – our spine is like any vertical structure, the more weight you carry, the harder the structure has to work to keep you upright, putting more stress on the tissue
- Core – your core muscles act as the support system for lumbar spine, if the core muscles are weak, the structure of the low back is more prone to injury
- Job – occupations with heavy and repetitive lifting have an increased risk of back problems
- Sport – certain sports such as weight-lifting, basketball, gymnastics, etc, can play a role in putting more force on the low back
- Lack of Activity – when you don’t move enough, the muscles of the core and lower back are not active, putting more pressure on the structure of the low back
- Smoking – there is evidence that tobacco use can weaken spinal tissue and accelerate the wearing of discs
Diagnosing Sciatica
Seeking medical professional who can take a proper history of the condition, is the most important aspect of diagnosing sciatica. At our office in Scarborough, we will take a thorough history of when the pain started and how it has progressed. We will then look at your posture, watch how you move and perform a variety of tests to confirm the diagnosis.
What are the symptoms of Sciatica?
- Severe Pain
- Muscle Weakness – in the Lower back, glutes, leg or feet
- Numbness and Tingling – in the legs, feet, toes
- Pain with sitting long periods
How can you tell the you have Sciatic pain versus non-specific Low Back Pain?
- Pain when coughing (valsalva’s test)
- Pain with flexion
- Duration of pain – if the pain lasts longer than 7 – 10 days
- Intensity of pain – the pain is more exquisite and intolerable
- Pain with straight leg raise
Valsalva Test
We will ask a patient to sit down, lean forward and pretend like they are blowing into a balloon (but use their knuckle as the balloon). This acts to increase pressure in the abdominal cavity and cause pain. If space is being taken up by a disc, this extra pressure will exert more force on the disc and cause pain.
Straight Leg Raise Test
We will ask the patient to lie on their back, and we will slowly raise their straightened leg towards the ceiling. If a disc is aggravated, they will usually experience pain around 60-70 degrees of the arc. This test acts to tension the nerve from the lower back to the foot, almost like pulling the extension cord behind your Television.
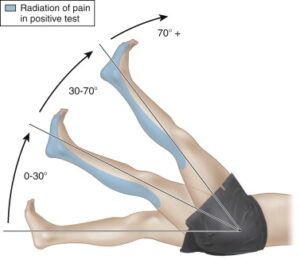
Figure 2. Straight Leg Raise Test
Neurological testing
We will perform a neurological exam on the patient, usually we will see a decrease in the reflexes of the patient. We will also check their muscle strength in their legs and feet, and if they have the same sensation on both sides of the legs. Depending on what level the disc is aggravated (usually between L4 and L5, or L5 and S1) they will have different symptoms.
L4 Nerve – symptoms will be felt on the upper thigh and inside shin
L5 Nerve – symptoms will be felt on the outside shin, top of the foot, and between the 1st and 2nd toes
S1 Nerve – symptoms will be felt down the back of the leg, ankle and bottom of the foot
See below for a chart of where you would see the respective symptoms.
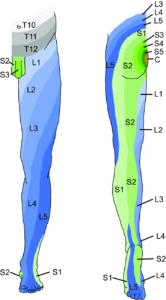
Figure 3. Lower Limb Dermatomes
Diagnostic Tests
It is important to understand that a clinical examination is the most important part of diagnosing a lumbar disc herniation and sciatica. However in severe cases where the pain is significant and not improving, more diagnostic tests are necessary.
X-Rays – imaging that targets the bone and looks for fractures, infections, tumours and bone spurts
MRI (Magnetic Resonance Imaging) – imaging that targets the soft tissues of the back. MRI’s can show discs, nerves and the spinal cord – this usually confirms sciatica as the diagnosis
Prognosis – What Can I Expect?
The majority of cases of sciatic pain go away with time and proper treatment. Approximately 80-90% of cases will get better within 4-8 weeks and without surgery.
For our next blog post, we are going to go over treatment and ultimately some strategies for prevention of sciatica in the future.
For more information read our other posts on low back pain, or read the links below:
Additional Resources:
Milner Chiropractic Clinic – Low Back Pain 101
https://milnerchiropractic.ca/what-to-know-if-you-have-lower-back-pain/
Ontario Chiropractic Association – Management of Back Pain
https://chiropractic.on.ca/self-management/seven-tips-to-get-your-back-on-track/
Cleveland Clinic – Sciatic Nerve Pain
https://my.clevelandclinic.org/health/diseases/12792-sciatica
Disclaimer – the content on this blog is designed for educational and information purposes only, it is not intended for medical advice. If you are in pain, call your medical professional.